Amphotericin B: Package Insert / Prescribing Info
Package insert / product label
Dosage form: injection, powder, lyophilized, for solution
Drug class: Polyenes
J Code (medical billing code): J0289 (10 mg, injection)
Medically reviewed by Drugs.com. Last updated on Nov 25, 2024.
On This Page
Amphotericin B Description
Amphotericin B liposome for injection is a sterile, non-pyrogenic, pale yellow to yellow lyophilized product for intravenous infusion. Each vial contains 50 mg of amphotericin B, USP, intercalated into a liposomal membrane consisting of approximately 0.64 mg alpha tocopherol, USP; 52 mg cholesterol, NF; 84 mg distearoyl phosphatidylglycerol, sodium salt; 213 mg hydrogenated soy phosphatidylcholine. In addition, 27 mg disodium succinate hexahydrate and 900 mg sucrose, NF are used as a buffer. Amphotericin B liposome for injection may contain hydrochloric acid and/or sodium hydroxide as pH adjusters. Following reconstitution with Sterile Water for Injection, USP, the resulting pH of the suspension is between 5 to 6.
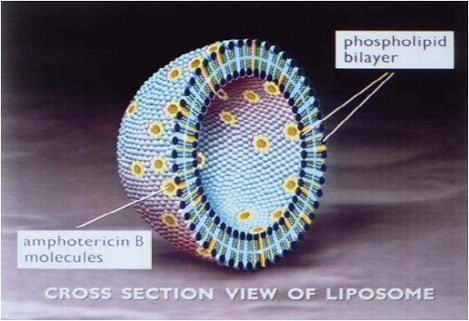
Amphotericin B liposome for injection is a true single bilayer liposomal drug delivery system. Liposomes are closed, spherical vesicles created by mixing specific proportions of amphophilic substances such as phospholipids and cholesterol so that they arrange themselves into multiple concentric bilayer membranes when hydrated in aqueous solutions. Single bilayer liposomes are then formed by microemulsification of multilamellar vesicles using a homogenizer. Amphotericin B liposome for injection consists of these unilamellar bilayer liposomes with amphotericin B intercalated within the membrane. Due to the nature and quantity of amphophilic substances used, and the lipophilic moiety in the amphotericin B molecule, the drug is an integral part of the overall structure of the amphotericin B liposome for injection liposomes. Amphotericin B liposome for injection contains true liposomes that are less than 100 nm in diameter. A schematic depiction of the liposome is presented below.
Note: Liposomal encapsulation or incorporation into a lipid complex can substantially affect a drug’s functional properties relative to those of the unencapsulated drug or non-lipid associated drug. In addition, different liposomal or lipid-complex products with a common active ingredient may vary from one another in the chemical composition and physical form of the lipid component. Such differences may affect the functional properties of these drug products.
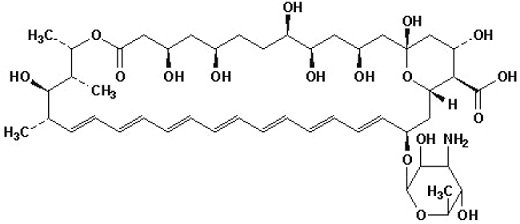
Amphotericin B is a macrocyclic, polyene, antifungal antibiotic produced from a strain of Streptomyces nodosus. Amphotericin B is designated chemically as: [1R-(1R*,3S*,5R*,6R*,9R*,11R*,15S*,16R*,17R*,18S*, 19E,21E,23E,25E,27E,29E,31E,33R*,35S*,36R*,37S*)]-33-[(3-Amino-3,6-dideoxy-β-D-mannopyranosyl)oxy]-1,3,5,6,9,11,17,37-octahydroxy-15,16,18-trimethyl-13-oxo-14,39-dioxabicyclo[33.3.1]nonatriaconta-19,21,23,25,27,29,31-heptaene-36-carboxylic acid (CAS No.1397-89-3).
Amphotericin B has a molecular formula of C47H73NO17 and a molecular weight of 924.08 g/mol.
The structure of amphotericin B is shown below:
MICROBIOLOGY
Mechanism of Action
Amphotericin B, the active ingredient of amphotericin B liposome for injection, acts by binding to the sterol component, ergosterol, of the cell membrane of susceptible fungi. It forms transmembrane channels leading to alterations in cell permeability through which monovalent ions (NA+, K+, H+, and Cl-) leak out of the cell resulting in cell death. While amphotericin B has a higher affinity for the ergosterol component of the fungal cell membrane, it can also bind to the cholesterol component of the mammalian cell leading to cytotoxicity. Amphotericin B liposome for injection, the liposomal preparation of amphotericin B, has been shown to penetrate the cell wall of both extracellular and intracellular forms of susceptible fungi.
Resistance
Mutants with decreased susceptibility to amphotericin B have been isolated from several fungal species after serial passage in culture media containing the drug, and from some patients receiving prolonged therapy. Drug combination studies in vitro and in vivo suggest that imidazoles may induce resistance to amphotericin B; however, the clinical relevance of drug resistance has not been established.
Antimicrobial Activity
Amphotericin B liposome for injection has shown in vitro activity comparable to amphotericin B against the following organisms: Aspergillus fumigatus, Aspergillus flavus, Candida albicans, Candida krusei, Candida lusitaniae, Candida parapsilosis, Candida tropicalis, Cryptococcus neoformans, and Blastomyces dermatitidis.
Susceptibility Testing
For specific information regarding susceptibility test interpretive criteria and associated test methods and quality control standards recognized by FDA for this drug, please see: https://www.fda.gov/STIC.
Amphotericin B - Clinical Pharmacology
Pharmacokinetics
The assay used to measure amphotericin B in the serum after administration of amphotericin B liposome for injection does not distinguish amphotericin B that is complexed with the phospholipids of amphotericin B liposome for injection from amphotericin B that is uncomplexed. The pharmacokinetic profile of amphotericin B after administration of amphotericin B liposome for injection is based upon total serum concentrations of amphotericin B. The pharmacokinetic profile of amphotericin B was determined in febrile neutropenic cancer and bone marrow transplant patients who received 1 to 2 hour infusions of 1 to 5 mg/kg/day amphotericin B liposome for injection for 3 to 20 days.
The pharmacokinetics of amphotericin B after administration of amphotericin B liposome for injection is nonlinear such that there is a greater than proportional increase in serum concentrations with an increase in dose from 1 to 5 mg/kg/day. The pharmacokinetic parameters of total amphotericin B (mean ± SD) after the first dose and at steady state are shown in the table below.
| Dose
| 1 mg/kg/day
| 2.5 mg/kg/day
| 5 mg/kg/day
|
|||||
| Day
| 1
N = 8 | Last
N = 7 | 1
N =7 | Last
N = 7 | 1
N = 12 | Last
N = 9 |
||
| Parameters
|
||||||||
| Cmax
(mcg/mL) | 7.3 ± 3.8 | 12.2 ± 4.9 | 17.2 ± 7.1 | 31.4 ± 17.8 | 57.6 ± 21 | 83 ± 35.2 |
||
| AUC0-24
(mcg·hr/mL) | 27 ± 14 | 60 ± 20 | 65 ± 33 | 197 ± 183 | 269 ± 96 | 555 ± 311 |
||
| t½(hr) | 10.7 ± 6.4 | 7 ± 2.1 | 8.1 ± 2.3 | 6.3 ± 2 | 6.4 ± 2.1 | 6.8 ± 2.1 |
||
| Vss(L/kg) | 0.44 ± 0.27 | 0.14 ± 0.05 | 0.40 ± 0.37 | 0.16 ± 0.09 | 0.16 ± 0.10 | 0.10 ± 0.07 |
||
| Cl (mL/hr/kg) | 39 ± 22 | 17 ± 6 | 51 ± 44 | 22 ± 15 | 21 ± 14 | 11 ± 6 |
||
Distribution
Based on total amphotericin B concentrations measured within a dosing interval (24 hours) after administration of amphotericin B liposome for injection, the mean half-life was 7 to 10 hours. However, based on total amphotericin B concentration measured up to 49 days after dosing of amphotericin B liposome for injection, the mean half-life was 100 to 153 hours. The long terminal elimination half-life is probably a slow redistribution from tissues. Steady state concentrations were generally achieved within 4 days of dosing.
Although variable, mean trough concentrations of amphotericin B remained relatively constant with repeated administration of the same dose over the range of 1 to 5 mg/kg/day, indicating no significant drug accumulation in the serum.
Metabolism
The metabolic pathways of amphotericin B after administration of amphotericin B liposome for injection are not known.
Excretion
The mean clearance at steady state was independent of dose. The excretion of amphotericin B after administration of amphotericin B liposome for injection has not been studied.
Pharmacokinetics in Special Populations
Renal Impairment
The effect of renal impairment on the disposition of amphotericin B after administration of amphotericin B liposome for injection has not been studied. However, amphotericin B liposome for injection has been successfully administered to patients with pre-existing renal impairment (see DESCRIPTION OF CLINICAL STUDIES).
Hepatic Impairment
The effect of hepatic impairment on the disposition of amphotericin B after administration of amphotericin B liposome for injection is not known.
Pediatric and Elderly Patients
The pharmacokinetics of amphotericin B after administration of amphotericin B liposome for injection in pediatric and elderly patients has not been studied; however, amphotericin B liposome for injection has been used in pediatric and elderly patients (see DESCRIPTION OF CLINICAL STUDIES).
Gender and Ethnicity
The effect of gender or ethnicity on the pharmacokinetics of amphotericin B after administration of amphotericin B liposome for injection is not known.
Indications and Usage for Amphotericin B
Amphotericin B liposome for injection is indicated for the following:
- Empirical therapy for presumed fungal infection in febrile, neutropenic patients.
- Treatment of Cryptococcal Meningitis in HIV-infected patients (see DESCRIPTION OF CLINICAL STUDIES).
- Treatment of patients with Aspergillus species, Candida species and/or Cryptococcus species infections (see above for the treatment of Cryptococcal Meningitis) refractory to amphotericin B deoxycholate, or in patients where renal impairment or unacceptable toxicity precludes the use of amphotericin B deoxycholate.
- Treatment of visceral leishmaniasis. In immunocompromised patients with visceral leishmaniasis treated with amphotericin B liposome for injection, relapse rates were high following initial clearance of parasites (see DESCRIPTION OF CLINICAL STUDIES).
See DOSAGE AND ADMINISTRATION for recommended doses by indication.
DESCRIPTION OF CLINICAL STUDIES
Eleven clinical studies supporting the efficacy and safety of amphotericin B were conducted. This clinical program included both controlled and uncontrolled studies. These studies, which involved 2,171 patients, included patients with confirmed systemic mycoses, empirical therapy, and visceral leishmaniasis.
Nineteen hundred and forty-six (1,946) episodes were evaluable for efficacy, of which 1,280 (302 pediatric and 978 adults) were treated with amphotericin B.
Three controlled empirical therapy trials compared the efficacy and safety of amphotericin B liposome for injection to amphotericin B. One of these studies was conducted in a pediatric population, one in adults, and a third in patients aged 2 years or more. In addition, a controlled empirical therapy trial comparing the safety of amphotericin B liposome for injection to Abelcet® (amphotericin B lipid complex) was conducted in patients aged 2 years or more.
One controlled trial compared the efficacy and safety of amphotericin B liposome for injection to amphotericin B in HIV patients with cryptococcal meningitis.
One compassionate use study enrolled patients who had failed amphotericin B deoxycholate therapy or who were unable to receive amphotericin B deoxycholate because of renal insufficiency.
Empirical Therapy in Febrile Neutropenic Patients
Study 94-0-002, a randomized, double-blind, comparative multi-center trial, evaluated the efficacy of amphotericin B liposome for injection (1.5 to 6 mg/kg/day) compared with amphotericin B deoxycholate (0.3 to 1.2 mg/kg/day) in the empirical treatment of 687 adult and pediatric neutropenic patients who were febrile despite having received at least 96 hours of broad spectrum antibacterial therapy. Therapeutic success required (a) resolution of fever during the neutropenic period, (b) absence of an emergent fungal infection, (c) patient survival for at least 7 days post therapy, (d) no discontinuation of therapy due to toxicity or lack of efficacy, and (e) resolution of any study-entry fungal infection.
The overall therapeutic success rates for amphotericin B liposome for injection and the amphotericin B deoxycholate were equivalent. Results are summarized in the following table. Note: The categories presented below are not mutually exclusive.
| * 8 and 10 patients, respectively, were treated as failures due to premature discontinuation alone. | ||
| | Amphotericin B Liposome for Injection 3 mg/kg/day | Amphotericin B 0.6 mg/kg/day |
| Number of patients receiving at least one dose of study drug | 343 | 344 |
| Overall Success | 171 (49.9%) | 169 (49.1%) |
| Fever resolution during neutropenic period | 199 (58%) | 200 (58.1%) |
| No treatment-emergent fungal infection | 300 (87.5%) | 301 (87.7%) |
| Survival through 7 days post study drug | 318 (92.7%) | 308 (89.5%) |
| Study drug not prematurely discontinued due to toxicity or lack of efficacy* | 294 (85.7%) | 280 (81.4%) |
This therapeutic equivalence had no apparent relationship to the use of prestudy antifungal prophylaxis or concomitant granulocytic colony-stimulating factors.
The incidence of mycologically-confirmed, and clinically-diagnosed, emergent fungal infections are presented in the following table. Amphotericin B liposome for injection and amphotericin B were found to be equivalent with respect to the total number of emergent fungal infections.
| | Amphotericin B Liposome for Injection 3 mg/kg/day | Amphotericin B 0.6 mg/kg/day |
| Number of patients receiving at least one dose of study drug | 343 | 344 |
| Mycologically-confirmed fungal infection | 11 (3.2%) | 27 (7.8%) |
| Clinically-diagnosed fungal infection | 32 (9.3%) | 16 (4.7%) |
| Total emergent fungal infections | 43 (12.5%) | 43 (12.5%) |
Mycologically-confirmed fungal infections at study entry were cured in 8 of 11 patients in the amphotericin B liposome for injection group and 7 of 10 in the amphotericin B group.
Study 97-0-034, a randomized, double-blind, comparative multi-center trial, evaluated the safety of amphotericin B liposome for injection (3 and 5 mg/kg/day) compared with amphotericin B lipid complex (5 mg/kg/day) in the empirical treatment of 202 adult and 42 pediatric neutropenic patients. One hundred and sixty-six (166) patients received amphotericin B liposome for injection (85 patients received 3 mg/kg/day and 81 received 5 mg/kg/day) and 78 patients received amphotericin B lipid complex. The study patients were febrile despite having received at least 72 hours of broad spectrum antibacterial therapy. The primary endpoint of this study was safety. The study was not designed to draw statistically meaningful conclusions related to comparative efficacy and, in fact, Abelcet is not labeled for this indication.
Two supportive, prospective, randomized, open-label, comparative multi-center studies examined the efficacy of two dosages of amphotericin B liposome for injection (1 and 3 mg/kg/day) compared to amphotericin B deoxycholate (1 mg/kg/day) in the treatment of neutropenic patients with presumed fungal infections. These patients were undergoing chemotherapy as part of a bone marrow transplant or had hematological disease. Study 104-10 enrolled adult patients (n=134). Study 104-14 enrolled pediatric patients (n=214). Both studies support the efficacy equivalence of amphotericin B liposome for injection and amphotericin B as empirical therapy in febrile neutropenic patients.
Treatment of Cryptococcal Meningitis in HIV-Infected Patients
Study 94-0-013, a randomized, double-blind, comparative multi-center trial, evaluated the efficacy of amphotericin B liposome for injection at doses (3 and 6 mg/kg/day) compared with amphotericin B deoxycholate (0.7 mg/kg/day) for the treatment of cryptococcal meningitis in 266 adult and one pediatric HIV-positive patients (the pediatric patient received amphotericin B deoxycholate). Of the 267 treated patients, 86 received amphotericin B liposome for injection 3 mg/kg/day, 94 received 6 mg/kg/day and 87 received amphotericin B deoxycholate; cryptococcal meningitis was documented by a positive CSF culture at baseline in 73, 85 and 76 patients, respectively. Patients received study drug once daily for an induction period of 11 to 21 days. Following induction, all patients were switched to oral fluconazole at 400 mg/day for adults and 200 mg/day for patients less than 13 years of age to complete 10 weeks of protocol-directed therapy. For mycologically evaluable patients, defined as all randomized patients who received at least one dose of study drug, had a positive baseline CSF culture, and had at least one follow-up culture, success was evaluated at week 2 (i.e., 14 ± 4 days), and was defined as CSF culture conversion. Success rates at 2 weeks for amphotericin B liposome for injection and amphotericin B deoxycholate are summarized in the following table:
| * 97.5% Confidence Interval for the difference between amphotericin B liposome for injection and amphotericin B success rates. A negative value is in favor of amphotericin B. A positive value is in favor of amphotericin B liposome for injection. | |||
| | Amphotericin B Liposome for Injection 3 mg/kg/day | Amphotericin B Liposome for Injection 6 mg/kg/day | Amphotericin B
0.7 mg/kg/day |
| Success at Week 2 | 35/60 (58.3%) 97.5% CI*= -9.4%, +31% | 36/75 (48%) 97.5% CI*= -18.8%, +19.8% | 29/61 (47.5 %) |
Success at 10 weeks was defined as clinical success at week 10 plus CSF culture conversion at or prior to week 10. Success rates at 10 weeks in patients with positive baseline culture for cryptococcus species are summarized in the following table and show that the efficacy of amphotericin B liposome for injection 6 mg/kg/day approximates the efficacy of the amphotericin B deoxycholate regimen. These data do not support the conclusion that amphotericin B liposome for injection 3 mg/kg/day is comparable in efficacy to amphotericin B deoxycholate. The table also presents 10-week survival rates for patients treated in this study.
| | Amphotericin B Liposome for Injection
3 mg/kg/day | Amphotericin B Liposome for Injection
6 mg/kg/day | Amphotericin B
0.7 mg/kg/day |
|---|---|---|---|
| * 97.5% Confidence Interval for the difference between amphotericin B liposome for injection and amphotericin B rates. A negative value is in favor of amphotericin B. A positive value is in favor of amphotericin B liposome for injection. | |||
| Success in patients with documented cryptococcal meningitis | 27/73 (37%) 97.5% CI* = -33.7%, +2.4% | 42/85 (49%) 97.5% CI* = -20.9%, +14.5% | 40/76 (53%) |
| Survival rates | 74/86 (86%) 97.5% CI* = -13.8%, +8.9% | 85/94 (90%) 97.5% CI* = -8.3%, +12.2% | 77/87 (89%) |
The incidence of infusion-related, cardiovascular and renal adverse events was lower in patients receiving amphotericin B liposome for injection compared to amphotericin B deoxycholate (see ADVERSE REACTIONS section for details); therefore, the risks and benefits (advantages and disadvantages) of the different amphotericin B formulations should be taken into consideration when selecting a patient treatment regimen.
Treatment of Patients with Aspergillus Species, Candida Species and/or Cryptococcus Species Infections Refractory to Amphotericin B Deoxycholate, or in Patients Where Renal Impairment or Unacceptable Toxicity Precludes the Use of Amphotericin B Deoxycholate
Amphotericin B liposome for injection was evaluated in a compassionate use study in hospitalized patients with systemic fungal infections. These patients either had fungal infections refractory to amphotericin B deoxycholate, were intolerant to the use of amphotericin B deoxycholate, or had pre-existing renal insufficiency. Patient recruitment involved 140 infectious episodes in 133 patients, with 53 episodes evaluable for mycological response and 91 episodes evaluable for clinical outcome. Clinical success and mycological eradication occurred in some patients with documented aspergillosis, candidiasis, and cryptococcosis.
Treatment of Visceral Leishmaniasis
Amphotericin B was studied in patients with visceral leishmaniasis who were infected in the Mediterranean basin with documented or presumed Leishmania infantum. Clinical studies have not provided conclusive data regarding efficacy against L. donovani or L. chagasi.
Amphotericin B achieved high rates of acute parasite clearance in immunocompetent patients when total doses of 12 to 30 mg/kg were administered. Most of these immunocompetent patients remained relapse-free during follow-up periods of 6 months or longer. While acute parasite clearance was achieved in most of the immunocompromised patients who received total doses of 30 to 40 mg/kg, the majority of these patients were observed to relapse in the 6 months following the completion of therapy. Of the 21 immunocompromised patients studied, 17 were coinfected with HIV; approximately half of the HIV-infected patients had AIDS. The following table presents a comparison of efficacy rates among immunocompetent and immunocompromised patients infected in the Mediterranean basin who had no prior treatment or remote prior treatment for visceral leishmaniasis. Efficacy is expressed as both acute parasite clearance at the end of therapy (EOT) and as overall success (clearance with no relapse) during the follow-up period (F/U) of greater than 6 months for immunocompetent and immunocompromised patients:
| Immunocompetent Patients
|
|||
| No. of Patients
| Parasite (%) Clearance at EOT
| Overall Success (%) at F/U
|
|
| 87 | 86/87 (98.9) | 83/86 (96.5) |
|
| Immunocompromised Patients
|
|||
| Regimen
| Total Dose
| Parasite (%) Clearance at EOT
| Overall Success (%) at F/U
|
| 100 mg/day X 21 days | 29 to 38.9 mg/kg | 10/10 (100) | 2/10 (20) |
| 4 mg/kg/day, days 1 to 5, and 10, 17, 24, 31, 38 | 40 mg/kg | 8/9 (88.9) | 0/7 (0) |
| TOTAL
| | 18/19 (94.7) | 2/17 (11.8) |
When followed for 6 months or more after treatment, the overall success rate among immunocompetent patients was 96.5% and the overall success rate among immunocompromised patients was 11.8% due to relapse in the majority of patients. While case reports have suggested there may be a role for long-term therapy to prevent relapses in HIV coinfected patients (Lopez-Dupla, et al. J Antimicrob Chemother 1993; 32: 657-659), there are no data to date documenting the efficacy or safety of repeat courses of amphotericin B or of maintenance therapy with this drug among immunocompromised patients.
Contraindications
Amphotericin B liposome for injection is contraindicated in those patients who have demonstrated or have a known hypersensitivity to amphotericin B deoxycholate or any other constituents of the product unless, in the opinion of the treating physician, the benefit of therapy outweighs the risk.
Warnings
Anaphylaxis has been reported with amphotericin B deoxycholate and other amphotericin B-containing drugs, including amphotericin B liposome for injection. If a severe anaphylactic reaction occurs, the infusion should be immediately discontinued and the patient should not receive further infusions of amphotericin B liposome for injection.
Precautions
General
As with any amphotericin B-containing product the drug should be administered by medically trained personnel. During the initial dosing period, patients should be under close clinical observation. Amphotericin B liposome for injection has been shown to be significantly less toxic than amphotericin B deoxycholate; however, adverse events may still occur.
Laboratory Tests
Patient management should include laboratory evaluation of renal, hepatic and hematopoietic function, and serum electrolytes (particularly magnesium and potassium).
Drug-Laboratory Interactions: Serum phosphate false elevation
False elevations of serum phosphate may occur when samples from patients receiving amphotericin B liposome for injection are analyzed using the PHOSm assay (e.g. used in Beckman Coulter analyzers including the Synchron LX20). This assay is intended for the quantitative determination of inorganic phosphorus in human serum, plasma or urine samples.
Drug Interactions
No formal clinical studies of drug interactions have been conducted with amphotericin B liposome for injection; however, the following drugs are known to interact with amphotericin B and may interact with amphotericin B liposome for injection:
Antineoplastic Agents
Concurrent use of antineoplastic agents may enhance the potential for renal toxicity, bronchospasm, and hypotension. Antineoplastic agents should be given concomitantly with caution.
Corticosteroids and Corticotropin (ACTH)
Concurrent use of corticosteroids and ACTH may potentiate hypokalemia, which could predispose the patient to cardiac dysfunction. If used concomitantly, serum electrolytes and cardiac function should be closely monitored.
Digitalis Glycosides
Concurrent use may induce hypokalemia and may potentiate digitalis toxicity. When administered concomitantly, serum potassium levels should be closely monitored.
Flucytosine
Concurrent use of flucytosine may increase the toxicity of flucytosine by possibly increasing its cellular uptake and/or impairing its renal excretion.
Azoles (e.g., ketoconazole, miconazole, clotrimazole, fluconazole, etc.)
In vitro and in vivo animal studies of the combination of amphotericin B and imidazoles suggest that imidazoles may induce fungal resistance to amphotericin B. Combination therapy should be administered with caution, especially in immunocompromised patients.
Leukocyte Transfusions
Acute pulmonary toxicity has been reported in patients simultaneously receiving intravenous amphotericin B and leukocyte transfusions.
Other Nephrotoxic Medications
Concurrent use of amphotericin B and other nephrotoxic medications may enhance the potential for drug-induced renal toxicity. Intensive monitoring of renal function is recommended in patients requiring any combination of nephrotoxic medications.
Skeletal Muscle Relaxants
Amphotericin B-induced hypokalemia may enhance the curariform effect of skeletal muscle relaxants (e.g. tubocurarine) due to hypokalemia. When administered concomitantly, serum potassium levels should be closely monitored.
Carcinogenesis, Mutagenesis, Impairment of Fertility
No long-term studies in animals have been performed to evaluate carcinogenic potential of amphotericin B liposome for injection. Amphotericin B liposome for injection has not been tested to determine its mutagenic potential. A Segment I Reproductive Study in rats found an abnormal estrous cycle (prolonged diestrus) and decreased number of corpora lutea in the high-dose groups (10 and 15 mg/kg, doses equivalent to human doses of 1.6 and 2.4 mg/kg based on body surface area considerations). Amphotericin B liposome for injection did not affect fertility or days to copulation. There were no effects on male reproductive function.
Pregnancy
There have been no adequate and well-controlled studies of amphotericin B liposome for injection in pregnant women. Systemic fungal infections have been successfully treated in pregnant women with amphotericin B deoxycholate, but the number of cases reported has been small.
Segment II studies in both rats and rabbits have concluded that amphotericin B liposome for injection had no teratogenic potential in these species. In rats, the maternal non-toxic dose of amphotericin B liposome for injection was estimated to be 5 mg/kg (equivalent to 0.16 to 0.8 times the recommended human clinical dose range of 1 to 5 mg/kg) and in rabbits, 3 mg/kg (equivalent to 0.2 to 1 times the recommended human clinical dose range), based on body surface area correction. Rabbits receiving the higher doses, (equivalent to 0.5 to 2 times the recommended human dose) of amphotericin B liposome for injection experienced a higher rate of spontaneous abortions than did the control groups. Amphotericin B liposome for injection should only be used during pregnancy if the possible benefits to be derived outweigh the potential risks involved.
Nursing Mothers
Many drugs are excreted in human milk; however, it is not known whether amphotericin B is excreted in human milk. Due to the potential for serious adverse reactions in breastfed infants, a decision should be made whether to discontinue nursing or whether to discontinue the drug, taking into account the importance of the drug to the mother.
Pediatric Use
Pediatric patients, age 1 month to 16 years, with presumed fungal infection (empirical therapy), confirmed systemic fungal infections or with visceral leishmaniasis have been successfully treated with amphotericin B liposome for injection. In studies which included 302 pediatric patients administered amphotericin B liposome for injection, there was no evidence of any differences in efficacy or safety of amphotericin B liposome for injection compared to adults. Since pediatric patients have received amphotericin B liposome for injection at doses comparable to those used in adults on a per kilogram body weight basis, no dosage adjustment is required in this population. Safety and effectiveness in pediatric patients below the age of one month have not been established (See DESCRIPTION OF CLINICAL STUDIES - Empirical Therapy in Febrile Neutropenic Patients and DOSAGE AND ADMINISTRATION).
Elderly Patients
Experience with amphotericin B liposome for injection in the elderly (65 years or older) comprised 72 patients. It has not been necessary to alter the dose of amphotericin B liposome for injection for this population. As with most other drugs, elderly patients receiving amphotericin B liposome for injection should be carefully monitored.
Adverse Reactions/Side Effects
The following adverse events are based on the experience of 592 adult patients (295 treated with amphotericin B liposome for injection and 297 treated with amphotericin B deoxycholate) and 95 pediatric patients (48 treated with amphotericin B liposome for injection and 47 treated with amphotericin B deoxycholate) in Study 94-0-002, a randomized double-blind, multi-center study in febrile, neutropenic patients. Amphotericin B liposome for injection and amphotericin B were infused over two hours.
The incidence of common adverse events (incidence of 10% or greater) occurring with amphotericin B liposome for injection compared to amphotericin B deoxycholate, regardless of relationship to study drug, is shown in the following table:
| Adverse Event by Body System
| Amphotericin B Liposome for Injection
N = 343 % | Amphotericin B
N = 344 % |
|---|---|---|
| Body as a Whole
|
||
| Abdominal pain | 19.8 | 21.8 |
| Asthenia | 13.1 | 10.8 |
| Back pain | 12 | 7.3 |
| Blood product transfusion reaction | 18.4 | 18.6 |
| Chills | 47.5 | 75.9 |
| Infection | 11.1 | 9.3 |
| Pain | 14 | 12.8 |
| Sepsis | 14 | 11.3 |
| Cardiovascular System
|
||
| Chest pain | 12 | 11.6 |
| Hypertension | 7.9 | 16.3 |
| Hypotension | 14.3 | 21.5 |
| Tachycardia | 13.4 | 20.9 |
| Digestive System
|
||
| Diarrhea | 30.3 | 27.3 |
| Gastrointestinal hemorrhage | 9.9 | 11.3 |
| Nausea | 39.7 | 38.7 |
| Vomiting | 31.8 | 43.9 |
| Metabolic and Nutritional Disorders
|
||
| Alkaline phosphatase increased | 22.2 | 19.2 |
| ALT (SGPT) increased | 14.6 | 14 |
| AST (SGOT) increased | 12.8 | 12.8 |
| Bilirubinemia | 18.1 | 19.2 |
| BUN increased | 21 | 31.1 |
| Creatinine increased | 22.4 | 42.2 |
| Edema | 14.3 | 14.8 |
| Hyperglycemia | 23 | 27.9 |
| Hypernatremia | 4.1 | 11 |
| Hypervolemia | 12.2 | 15.4 |
| Hypocalcemia | 18.4 | 20.9 |
| Hypokalemia | 42.9 | 50.6 |
| Hypomagnesemia | 20.4 | 25.6 |
| Peripheral edema | 14.6 | 17.2 |
| Nervous System
|
||
| Anxiety | 13.7 | 11 |
| Confusion | 11.4 | 13.4 |
| Headache | 19.8 | 20.9 |
| Insomnia | 17.2 | 14.2 |
| Respiratory System
|
||
| Cough increased | 17.8 | 21.8 |
| Dyspnea | 23 | 29.1 |
| Epistaxis | 14.9 | 20.1 |
| Hypoxia | 7.6 | 14.8 |
| Lung disorder | 17.8 | 17.4 |
| Pleural effusion | 12.5 | 9.6 |
| Rhinitis | 11.1 | 11 |
| Skin and Appendages
|
||
| Pruritus | 10.8 | 10.2 |
| Rash | 24.8 | 24.4 |
| Sweating | 7 | 10.8 |
| Urogenital System
|
||
| Hematuria | 14 | 14 |
Amphotericin B liposome for injection was well tolerated. Amphotericin B liposome for injection had a lower incidence of chills, hypertension, hypotension, tachycardia, hypoxia, hypokalemia, and various events related to decreased kidney function as compared to amphotericin B deoxycholate.
In pediatric patients (16 years of age or less) in this double-blind study, amphotericin B liposome for injection compared to amphotericin B deoxycholate, had a lower incidence of hypokalemia (37% versus 55%), chills (29% versus 68%), vomiting (27% versus 55%), and hypertension (10% versus 21%). Similar trends, although with a somewhat lower incidence, were observed in open-label, randomized Study 104-14 involving 205 febrile neutropenic pediatric patients (141 treated with amphotericin B liposome for injection and 64 treated with amphotericin B deoxycholate). Pediatric patients appear to have more tolerance than older individuals for the nephrotoxic effects of amphotericin B deoxycholate.
The following adverse events are based on the experience of 244 patients (202 adult and 42 pediatric patients) of whom 85 patients were treated with amphotericin B liposome for injection 3 mg/kg, 81 patients were treated with amphotericin B liposome for injection 5 mg/kg and 78 patients were treated with amphotericin B lipid complex 5 mg/kg in Study 97-0-034, a randomized, double-blind, multi-center study in febrile, neutropenic patients. Amphotericin B liposome for injection and amphotericin B lipid complex were infused over two hours. The incidence of adverse events occurring in more than 10% of subjects in one or more arms, regardless of relationship to study drug, are summarized in the following table:
| Adverse Event by Body System
| Amphotericin B Liposome for Injection
3 mg/kg/day N = 85 % | Amphotericin B Liposome for Injection
5 mg/kg/day N = 81 % | Amphotericin B Lipid Complex
5 mg/kg/day N = 78 % |
|---|---|---|---|
| Body as a Whole
|
|||
| Abdominal pain | 12.9 | 9.9 | 11.5 |
| Asthenia | 8.2 | 6.2 | 11.5 |
| Chills/rigors | 40 | 48.1 | 89.7 |
| Sepsis | 12.9 | 7.4 | 11.5 |
| Transfusion reaction | 10.6 | 8.6 | 5.1 |
| Cardiovascular System
|
|||
| Chest pain | 8.2 | 11.1 | 6.4 |
| Hypertension | 10.6 | 19.8 | 23.1 |
| Hypotension | 10.6 | 7.4 | 19.2 |
| Tachycardia | 9.4 | 18.5 | 23.1 |
| Digestive System
|
|||
| Diarrhea | 15.3 | 17.3 | 14.1 |
| Nausea | 25.9 | 29.6 | 37.2 |
| Vomiting | 22.4 | 25.9 | 30.8 |
| Metabolic and Nutritional Disorders
|
|||
| Alkaline phosphatase increased | 7.1 | 8.6 | 12.8 |
| Bilirubinemia | 16.5 | 11.1 | 11.5 |
| BUN increased | 20 | 18.5 | 28.2 |
| Creatinine increased | 20 | 18.5 | 48.7 |
| Edema | 12.9 | 12.3 | 12.8 |
| Hyperglycemia | 8.2 | 8.6 | 14.1 |
| Hypervolemia | 8.2 | 11.1 | 14.1 |
| Hypocalcemia | 10.6 | 4.9 | 5.1 |
| Hypokalemia | 37.6 | 43.2 | 39.7 |
| Hypomagnesemia | 15.3 | 25.9 | 15.4 |
| Liver function tests abnormal | 10.6 | 7.4 | 11.5 |
| Nervous System
|
|||
| Anxiety | 10.6 | 7.4 | 9 |
| Confusion | 12.9 | 8.6 | 3.8 |
| Headache | 9.4 | 17.3 | 10.3 |
| Respiratory System
|
|||
| Dyspnea | 17.6 | 22.2 | 23.1 |
| Epistaxis | 10.6 | 8.6 | 14.1 |
| Hypoxia | 7.1 | 6.2 | 20.5 |
| Lung disorder | 14.1 | 13.6 | 15.4 |
| Skin and Appendages
|
|||
| Rash | 23.5 | 22.2 | 14.1 |
The following adverse events are based on the experience of 267 patients (266 adult patients and 1 pediatric patient) of whom 86 patients were treated with amphotericin B liposome for injection 3 mg/kg, 94 patients were treated with amphotericin B liposome for injection 6 mg/kg and 87 patients were treated with amphotericin B deoxycholate 0.7 mg/kg in Study 94-0-013 a randomized, double-blind, comparative multi-center trial, in the treatment of cryptococcal meningitis in HIV-positive patients. The incidence of adverse events occurring in more than 10% of subjects in one or more arms regardless of relationship to study drug are summarized in the following table:
| Adverse Event by Body System
| Amphotericin B Liposome for Injection
3 mg/kg/day N = 86 % | Amphotericin B Liposome for Injection
6 mg/kg/day N = 94 % | Amphotericin B
0.7 mg/kg/day N = 87 % |
|---|---|---|---|
| Body as a Whole
|
|||
| Abdominal pain | 7 | 7.4 | 10.3 |
| Infection | 12.8 | 11.7 | 6.9 |
| Procedural Complication | 8.1 | 9.6 | 10.3 |
| Cardiovascular System
|
|||
| Phlebitis | 9.3 | 10.6 | 25.3 |
| Digestive System
|
|||
| Anorexia | 14 | 9.6 | 11.5 |
| Constipation | 15.1 | 14.9 | 20.7 |
| Diarrhea | 10.5 | 16 | 10.3 |
| Nausea | 16.3 | 21.3 | 25.3 |
| Vomiting | 10.5 | 21.3 | 20.7 |
| Hemic and Lymphatic System
|
|||
| Anemia | 26.7 | 47.9 | 43.7 |
| Leukopenia | 15.1 | 17 | 17.2 |
| Thrombocytopenia | 5.8 | 12.8 | 6.9 |
| Metabolic and Nutritional Disorders
|
|||
| Bilirubinemia | 0 | 8.5 | 12.6 |
| BUN increased | 9.3 | 7.4 | 10.3 |
| Creatinine increased | 18.6 | 39.4 | 43.7 |
| Hyperglycemia | 9.3 | 12.8 | 17.2 |
| Hypocalcemia | 12.8 | 17 | 13.8 |
| Hypokalemia | 31.4 | 51.1 | 48.3 |
| Hypomagnesemia | 29.1 | 48.9 | 40.2 |
| Hyponatremia | 11.6 | 8.5 | 9.2 |
| Liver Function Tests Abnormal | 12.8 | 4.3 | 9.2 |
| Nervous System
|
|||
| Dizziness | 7 | 8.5 | 10.3 |
| Insomnia | 22.1 | 17 | 20.7 |
| Respiratory System
|
|||
| Cough Increased | 8.1 | 2.1 | 10.3 |
| Skin and Appendages
|
|||
| Rash | 4.7 | 11.7 | 4.6 |
Infusion-Related Reactions
In Study 94-0-002, the large, double-blind study of pediatric and adult febrile neutropenic patients, no premedication to prevent infusion-related reaction was administered prior to the first dose of study drug (Day 1). Amphotericin B liposome for injection-treated patients had a lower incidence of infusion-related fever (17% versus 44%), chills/rigors (18% versus 54%) and vomiting (6% versus 8%) on Day 1 as compared to amphotericin B deoxycholate-treated patients.
The incidence of infusion-related reactions on Day 1 in pediatric and adult patients is summarized in the following table:
| * Day 1 body temperature increased above the temperature taken within 1 hour prior to infusion (preinfusion temperature) or above the lowest infusion value (no preinfusion temperature recorded). | ||||
| | Pediatric Patients
(≤ 16 years of age) | Adult Patients
(>16 years of age) |
||
| | Amphotericin B Liposome for Injection 3 mg/kg/day | Amphotericin B 0.6 mg/kg/day | Amphotericin B Liposome for Injection 3 mg/kg/day | Amphotericin B 0.6 mg/kg/day |
| Total number of patients receiving at least one dose of study drug | 48 | 47 | 295 | 297 |
| Patients with fever* increase ≥1.0ºC | 6 (13%) | 22 (47%) | 52 (18%) | 128 (43%) |
| Patients with chills/rigors | 4 (8%) | 22 (47%) | 59 (20%) | 165 (56%) |
| Patients with nausea | 4 (8%) | 4 (9%) | 38 (13%) | 31 (10%) |
| Patients with vomiting | 2 (4%) | 7 (15%) | 19 (6%) | 21 (7%) |
| Patients with other reactions | 10 (21%) | 13 (28%) | 47 (16%) | 69 (23%) |
Cardiorespiratory events, except for vasodilatation (flushing), during all study drug infusions were more frequent in amphotericin B-treated patients as summarized in the following table:
| Event
| Amphotericin B Liposome for Injection 3 mg/kg/day N = 343 | Amphotericin B 0.6 mg/kg/day N = 344 |
| Hypotension | 12 (3.5%) | 28 (8.1%) |
| Tachycardia | 8 (2.3%) | 43 (12.5%) |
| Hypertension | 8 (2.3%) | 39 (11.3%) |
| Vasodilatation | 18 (5.2%) | 2 (0.6%) |
| Dyspnea | 16 (4.7%) | 25 (7.3%) |
| Hyperventilation | 4 (1.2%) | 17 (4.9%) |
| Hypoxia | 1 (0.3%) | 22 (6.4%) |
The percentage of patients who received drugs either for the treatment or prevention of infusion-related reactions (e.g., acetaminophen, diphenhydramine, meperidine and hydrocortisone) was lower in amphotericin B liposome for injection-treated patients compared with amphotericin B deoxycholate-treated patients.
In the empirical therapy study 97-0-034, on Day 1, where no premedication was administered, the overall incidence of infusion-related events of chills/rigors was significantly lower for patients administered amphotericin B liposome for injection compared with amphotericin B lipid complex. Fever, chills/rigors and hypoxia were significantly lower for each amphotericin B liposome for injection group compared with the amphotericin B lipid complex group. The infusion-related event hypoxia was reported for 11.5% of amphotericin B lipid complex-treated patients compared with 0% of patients administered 3 mg/kg per day amphotericin B liposome for injection and 1.2% of patients treated with 5 mg/kg per day amphotericin B liposome for injection.
| | Amphotericin B Liposome for Injection
| Amphotericin B lipid complex
5 mg/kg/day |
||
| 3 mg/kg/day
| 5 mg/kg/day
| BOTH
|
||
| Total number of patients | 85 | 81 | 166 | 78 |
| Patients with Chills/Rigors (Day 1) | 16 (18.8%) | 19 (23.5%) | 35 (21.1%) | 62 (79.5%) |
| Patients with other notable reactions: |
||||
| Fever (≥1.0ºC increase in temperature) | 20 (23.5%) | 16 (19.8%) | 36 (21.7%) | 45 (57.7%) |
| Nausea | 9 (10.6%) | 7 (8.6%) | 16 (9.6%) | 9 (11.5%) |
| Vomiting | 5 (5.9%) | 5 (6.2%) | 10 (6%) | 11 (14.1%) |
| Hypertension | 4 (4.7%) | 7 (8.6%) | 11 (6.6%) | 12 (15.4%) |
| Tachycardia | 2 (2.4%) | 8 (9.9%) | 10 (6%) | 14 (17.9%) |
| Dyspnea | 4 (4.7%) | 8 (9.9%) | 12 (7.2%) | 8 (10.3%) |
| Hypoxia | 0 | 1 (1.2%) | 1 (<1%) | 9 (11.5%) |
Day 1 body temperature increased above the temperature taken within 1 hour prior to infusion (preinfusion temperature) or above the lowest infusion value (no preinfusion temperature recorded).
Patients were not administered premedications to prevent infusion-related reactions prior to the Day 1 study drug infusion.
In Study 94-0-013, a randomized, double-blind, multicenter trial comparing amphotericin B liposome for injection and amphotericin B deoxycholate as initial therapy for cryptococcal meningitis, premedications to prevent infusion-related reactions were permitted. Amphotericin B liposome for injection-treated patients had a lower incidence of fever, chills/rigors and respiratory adverse events as summarized in the following table:
| | Amphotericin B Liposome for Injection 3 mg/kg/day | Amphotericin B Liposome for Injection 6 mg/kg/day | Amphotericin B 0.7 mg/kg/day |
| Total number of patients receiving at least one dose of study drug | 86 | 94 | 87 |
| Patients with fever increase of >1°C | 6 (7%) | 8 (9%) | 24 (28%) |
| Patients with chills/rigors | 5 (6%) | 8 (9%) | 42 (48%) |
| Patients with nausea | 11 (13%) | 13 (14%) | 18 (20%) |
| Patients with vomiting | 14 (16%) | 13 (14%) | 16 (18%) |
| Respiratory adverse events | 0 | 1 (1%) | 8 (9%) |
There have been a few reports of flushing, back pain with or without chest tightness, and chest pain associated with amphotericin B liposome for injection administration; on occasion this has been severe. Where these symptoms were noted, the reaction developed within a few minutes after the start of infusion and disappeared rapidly when the infusion was stopped. The symptoms do not occur with every dose and usually do not recur on subsequent administrations when the infusion rate is slowed.
Toxicity and Discontinuation of Dosing
In Study 94-0-002, a significantly lower incidence of grade 3 or 4 toxicity was observed in the amphotericin B liposome for injection group compared with the amphotericin B group. In addition, nearly three times as many patients administered amphotericin B required a reduction in dose due to toxicity or discontinuation of study drug due to an infusion-related reaction compared with those administered amphotericin B liposome for injection.
In empirical therapy study 97-0-034, a greater proportion of patients in the amphotericin B lipid complex group discontinued the study drug due to an adverse event than in the amphotericin B liposome for injection groups.
Less Common Adverse Events
The following adverse events also have been reported in 2% to 10% of amphotericin B liposome for injection-treated patients receiving chemotherapy or bone marrow transplantation, or who had HIV disease in six comparative, clinical trials:
Body as a Whole
Abdomen enlarged, allergic reaction, cellulitis, cell-mediated immunological reaction, face edema, graft-versus-host disease, malaise, neck pain, and procedural complication.
Cardiovascular System
Arrhythmia, atrial fibrillation, bradycardia, cardiac arrest, cardiomegaly, hemorrhage, postural hypotension, valvular heart disease, vascular disorder, and vasodilatation (flushing).
Digestive System
Anorexia, constipation, dry mouth/nose, dyspepsia, dysphagia, eructation, fecal incontinence, flatulence, hemorrhoids, gum/oral hemorrhage, hematemesis, hepatocellular damage, hepatomegaly, liver function test abnormal, ileus, mucositis, rectal disorder, stomatitis, ulcerative stomatitis, and veno-occlusive liver disease.
Hemic & Lymphatic System
Anemia, coagulation disorder, ecchymosis, fluid overload, petechia, prothrombin decreased, prothrombin increased, and thrombocytopenia.
Metabolic & Nutritional Disorders
Acidosis, amylase increased, hyperchloremia, hyperkalemia, hypermagnesemia, hyperphosphatemia, hyponatremia, hypophosphatemia, hypoproteinemia, lactate dehydrogenase increased, nonprotein nitrogen (NPN) increased, and respiratory alkalosis.
Musculoskeletal System
Arthralgia, bone pain, dystonia, myalgia, and rigors.
Nervous System
Agitation, coma, convulsion, cough, depression, dysesthesia, dizziness, hallucinations, nervousness, paresthesia, somnolence, thinking abnormality, and tremor.
Respiratory System
Asthma, atelectasis, hemoptysis, hiccup, hyperventilation, influenza-like symptoms, lung edema, pharyngitis, pneumonia, respiratory insufficiency, respiratory failure, and sinusitis.
Skin & Appendages
Alopecia, dry skin, herpes simplex, injection site inflammation, maculopapular rash, purpura, skin discoloration, skin disorder, skin ulcer, urticaria, and vesiculobullous rash.
Special Senses
Conjunctivitis, dry eyes, and eye hemorrhage.
Urogenital System
Abnormal renal function, acute kidney failure, acute renal failure, dysuria, kidney failure, toxic nephropathy, urinary incontinence, and vaginal hemorrhage.
Post-marketing Experience
The following infrequent adverse experiences have been reported in post-marketing surveillance, in addition to those mentioned above: angioedema, erythema, urticaria, bronchospasm, cyanosis/hypoventilation, pulmonary edema, agranulocytosis, hemorrhagic cystitis, and rhabdomyolysis.
Clinical Laboratory Values
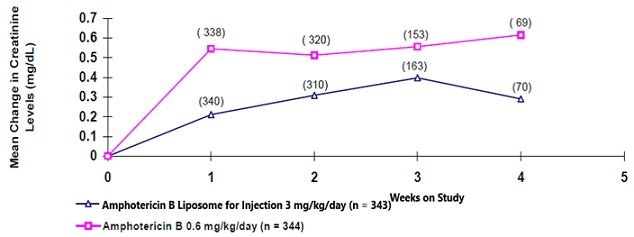
The effect of amphotericin B liposome for injection on renal and hepatic function and on serum electrolytes was assessed from laboratory values measured repeatedly in Study 94-0-002. The frequency and magnitude of hepatic test abnormalities were similar in the amphotericin B liposome for injection and amphotericin B groups. Nephrotoxicity was defined as creatinine values increasing 100% or more over pretreatment levels in pediatric patients, and creatinine values increasing 100% or more over pretreatment levels in adult patients, provided the peak creatinine concentration was >1.2 mg/dL. Hypokalemia was defined as potassium levels ≤ 2.5 mmol/L any time during treatment.
Incidence of nephrotoxicity, mean peak serum creatinine concentration, mean change from baseline in serum creatinine, and incidence of hypokalemia in the double-blind, randomized study were lower in the amphotericin B liposome for injection group as summarized in the following table:
| | Amphotericin B Liposome for Injection 3 mg/kg/day | Amphotericin B 0.6 mg/kg/day |
| Total number of patients receiving at least one dose of study drug | 343 | 344 |
| Nephrotoxicity | 64 (18.7%) | 116 (33.7%) |
| Mean peak creatinine | 1.24 mg/dL | 1.52 mg/dL |
| Mean change from baseline in creatinine | 0.48 mg/dL | 0.77 mg/dL |
| Hypokalemia | 23 (6.7%) | 40 (11.6%) |
The effect of amphotericin B liposome for injection (3 mg/kg/day) vs. amphotericin B (0.6 mg/kg/day) on renal function in adult patients enrolled in this study is illustrated in the following figure:
Mean Change in Creatinine Over Time in Study 94-0-002
In empirical therapy study 97-0-034, the incidence of nephrotoxicity as measured by increases of serum creatinine from baseline was significantly lower for patients administered amphotericin B liposome for injection (individual dose groups and combined) compared with amphotericin B lipid complex.
| | Amphotericin B Liposome for Injection
| Amphotericin B lipid complex
5 mg/kg/day |
||
| 3 mg/kg/day
| 5 mg/kg/day
| BOTH
|
||
| Total number of patients | 85 | 81 | 166 | 78 |
| Number with nephrotoxicity |
||||
| 1.5X baseline serum creatinine value | 25 (29.4%) | 21 (25.9%) | 46 (27.7%) | 49 (62.8%) |
| 2X baseline serum creatinine value | 12 (14.1%) | 12 (14.8%) | 24 (14.5%) | 33 (42.3%) |
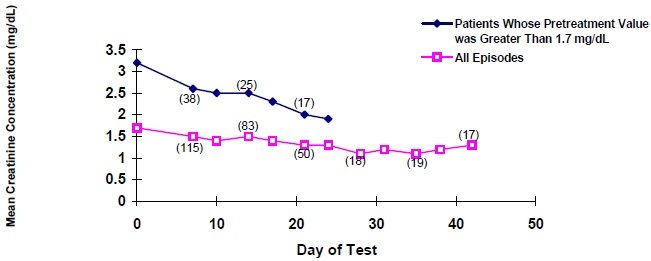
The following graph shows the average serum creatinine concentrations in the compassionate use study and shows that there is a drop from pretreatment concentrations for all patients, especially those with elevated (greater than 1.7 mg/dL) pretreatment creatinine concentrations.
Mean Creatinine Concentrations Over Time
The incidence of nephrotoxicity in Study 94-0-013 comparative trial in cryptococcal meningitis was lower in the amphotericin B liposome for injection groups as shown in the following table:
| | Amphotericin B Liposome for Injection
3 mg/kg/day | Amphotericin B Liposome for Injection
6 mg/kg/day | Amphotericin B 0.7 mg/kg/day |
| Total number of patients receiving at least one dose of study drug | 86 | 94 | 87 |
| Number with Nephrotoxicity (%) |
|||
| 1.5X baseline serum creatinine | 30 (35%) | 44 (47%) | 52 (60%) |
| 2X baseline serum creatinine | 12 (14%) | 20 (21%) | 29 (33%) |
Overdosage
The toxicity of amphotericin B liposome for injection due to overdose has not been defined. Repeated daily doses up to 10 mg/kg in pediatric patients and 15 mg/kg in adult patients have been administered in clinical trials with no reported dose-related toxicity.
Management
If overdosage should occur, cease administration immediately. Symptomatic supportive measures should be instituted. Particular attention should be given to monitoring renal function. Hemodialysis or peritoneal dialysis do not appear to significantly affect the elimination of amphotericin B liposome for injection.
Amphotericin B Dosage and Administration
Amphotericin B liposome for injection is not interchangeable or substitutable on a mg per mg basis with other amphotericin B products. Different amphotericin B products are not equivalent in terms of pharmacodynamics, pharmacokinetics and dosing.
Amphotericin B liposome for injection should be administered by intravenous infusion, using a controlled infusion device, over a period of approximately 120 minutes.
An in-line membrane filter may be used for the intravenous infusion of amphotericin B liposome for injection, provided THE MEAN PORE DIAMETER OF THE FILTER IS NOT LESS THAN 1.0 MICRON.
NOTE: An existing intravenous line must be flushed with 5% Dextrose Injection prior to infusion of amphotericin B liposome for injection. If this is not feasible, amphotericin B liposome for injection must be administered through a separate line.
Infusion time may be reduced to approximately 60 minutes in patients in whom the treatment is well-tolerated. If the patient experiences discomfort during infusion, the duration of infusion may be increased.
The recommended initial dose of amphotericin B liposome for injection for each indication for adult and pediatric patients is as follows:
| Indication
| Dose (mg/kg/day)
|
| Empirical therapy | 3 |
| Systemic fungal infections: Aspergillus Candida Cryptococcus | 3 to 5 |
| Cryptococcal meningitis in HIV-infected patients (see DESCRIPTION OF CLINICAL STUDIES) | 6 |
Dosing and rate of infusion should be individualized to the needs of the specific patient to ensure maximum efficacy while minimizing systemic toxicities or adverse events.
Doses recommended for visceral leishmaniasis are presented below:
| Visceral Leishmaniasis
| Dose (mg/kg/day)
|
| Immunocompetent patients | 3 (days 1 to 5) and 3 on days 14, 21 |
| Immunocompromised patients | 4 (days 1 to 5) and 4 on days 10, 17, 24, 31, 38 |
For immunocompetent patients who do not achieve parasitic clearance with the recommended dose, a repeat course of therapy may be useful.
For immunocompromised patients who do not clear parasites or who experience relapses, expert advice regarding further treatment is recommended. For additional information, see DESCRIPTION OF CLINICAL STUDIES.
Directions for Reconstitution, Filtration and Dilution
Read This Entire Section Carefully Before Beginning Reconstitution
Amphotericin B liposome for injection must be reconstituted using Sterile Water for Injection, USP (without a bacteriostatic agent). Vials of amphotericin B liposome for injection containing 50 mg of amphotericin B are prepared as follows:
Reconstitution
1. Aseptically add 12 mL of Sterile Water for Injection, USP to each amphotericin B liposome for injection vial to yield a preparation containing 4 mg amphotericin B/mL.
CAUTION: DO NOT RECONSTITUTE WITH SALINE OR ADD SALINE TO THE RECONSTITUTED CONCENTRATION, OR MIX WITH OTHER DRUGS. The use of any solution other than those recommended, or the presence of a bacteriostatic agent in the solution, may cause precipitation of amphotericin B liposome for injection.
2. Immediately after the addition of water, SHAKE THE VIAL VIGOROUSLY for 30 seconds to completely disperse the amphotericin B liposome for injection. Amphotericin B liposome for injection forms a yellow translucent suspension. Visually inspect the vial for particulate matter and continue shaking until completely dispersed.
Filtration and Dilution
3. Calculate the amount of reconstituted (4 mg/mL) amphotericin B liposome for injection to be further diluted.
4. Withdraw this amount of reconstituted amphotericin B liposome for injection into a sterile syringe.
5. Attach the 5 micron filter provided to the syringe. Inject the syringe contents through the filter, into the appropriate amount of 5% Dextrose Injection (use only one filter per vial of amphotericin B liposome for injection).
6. Amphotericin B liposome for injection must be diluted with 5% Dextrose Injection to a final concentration of 1 to 2 mg/mL prior to administration. Lower concentrations (0.2 to 0.5 mg/mL) may be appropriate for infants and small children to provide sufficient volume for infusion. DISCARD PARTIALLY USED VIALS.
STORAGE OF AMPHOTERICIN B LIPOSOME FOR INJECTION
Unopened vials of lyophilized material are to be stored at temperatures up to 25° C (77° F).
Storage of Reconstituted Product Concentrate
The reconstituted product concentrate may be stored for up to 24 hours at 2° to 8°C (36° to 46°F) following reconstitution with Sterile Water for Injection, USP. Do not freeze.
Storage of Diluted Product
Injection of amphotericin B liposome for injection should commence within 6 hours of dilution with 5% Dextrose Injection.
As with all parenteral drug products, the reconstituted amphotericin B liposome for injection should be inspected visually for particulate matter and discoloration prior to administration, whenever solution and container permit. Do not use material if there is any evidence of precipitation or foreign matter. Aseptic technique must be strictly observed in all handling, since no preservative or bacteriostatic agent is present in amphotericin B liposome for injection or in the materials specified for reconstitution and dilution.
How is Amphotericin B supplied
Amphotericin B liposome for injection is pale yellow to yellow lyophilized product, available as single cartons.
50 mg per Vial
Single-dose vial
Packaged individually NDC 55150-365-01
Each carton contains one pre-packaged, disposable sterile 5 micron filter.
The vial stopper is not made with natural rubber latex.
All brands listed are the trademarks of their respective owners and are not trademarks of Eugia Pharma Specialities Limited.
Distributed by:
Eugia US LLC
279 Princeton-Hightstown Rd.
E. Windsor, NJ 08520
Manufactured by:
TTY Biopharm Company Limited LiouDu Factory
No. 5 Gongjian West Road, Qidu District,
Keelung City, 20647, Taiwan
Revised: September 2022
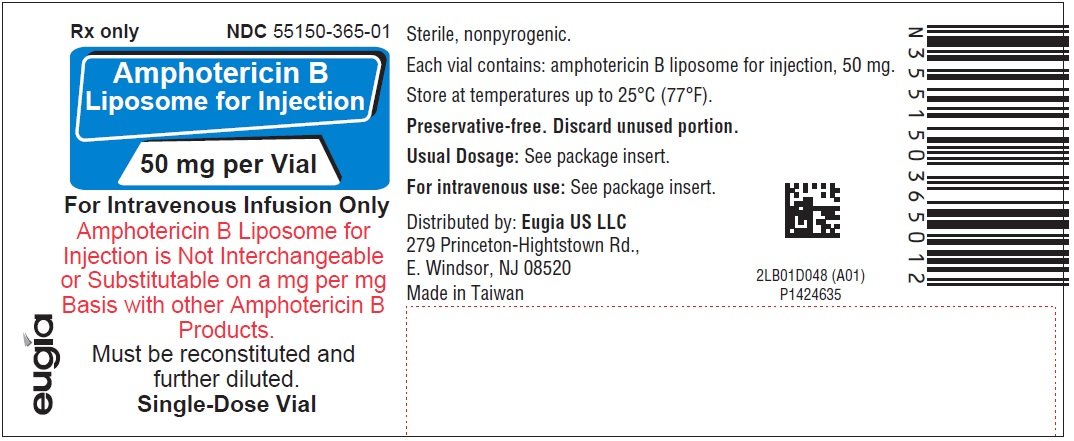
PACKAGE LABEL-PRINCIPAL DISPLAY PANEL-50 mg per Vial - Container Label
Rx only NDC 55150-365-01
Amphotericin B
Liposome for Injection
50 mg per Vial
For Intravenous Infusion Only
Amphotericin B Liposome for
Injection is Not Interchangeable
or Substitutable on a mg per mg
Basic with other Amphotericin B
Products.
Must be reconstituted and
further diluted.
Single-Dose Vial
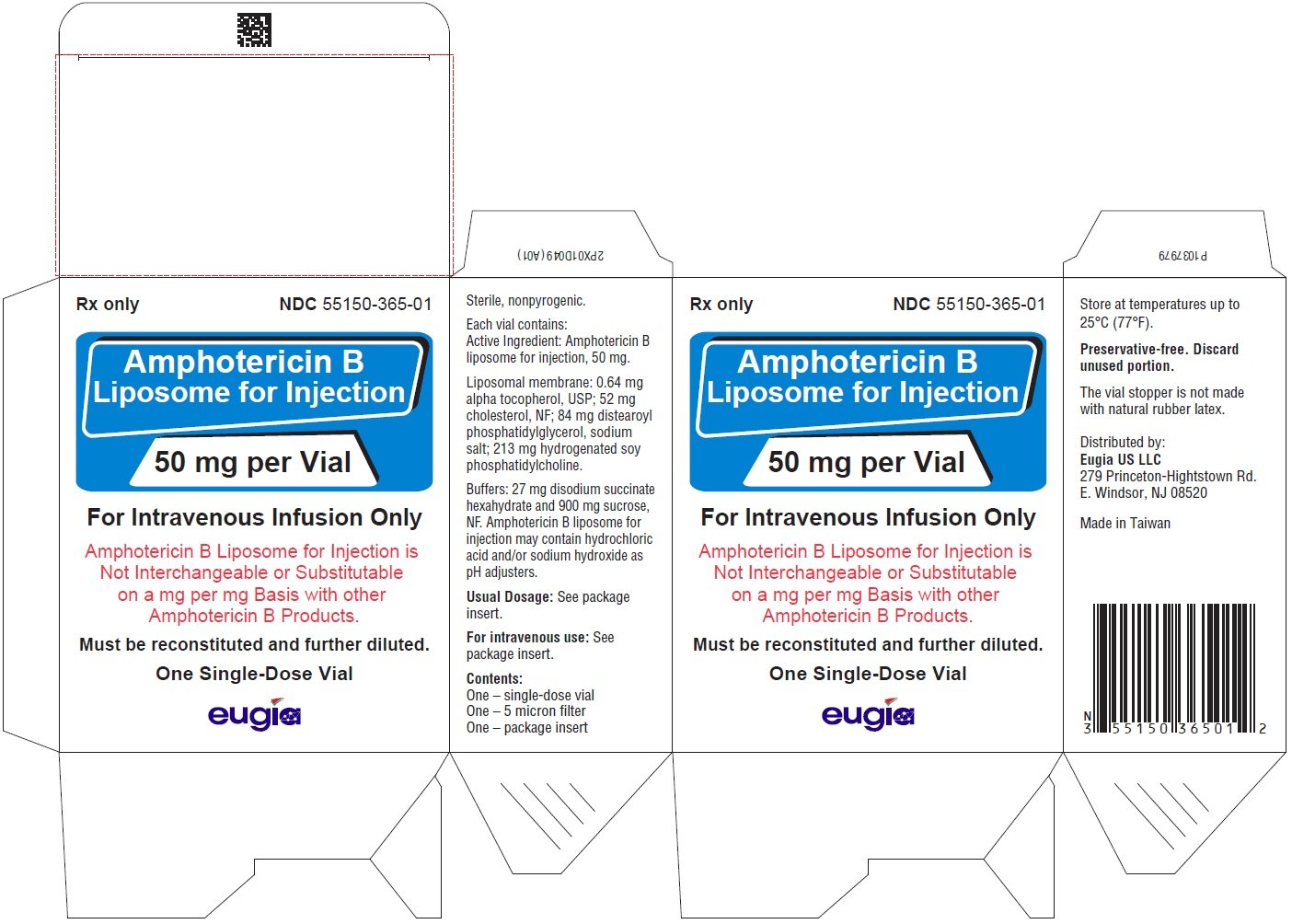
PACKAGE LABEL-PRINCIPAL DISPLAY PANEL-50 mg per Vial - Container-Carton (1 Vial)
Rx only NDC 55150-365-01
Amphotericin B
Liposome for Injection
50 mg per Vial
For Intravenous Infusion Only
Amphotericin B Liposome for Injection is
Not Interchangeable or Substitutable
on a mg per mg Basis with other
Amphotericin B Products.
Must be reconstituted and further diluted.
One Single-Dose Vial
eugia
| AMPHOTERICIN B
amphotericin b injection, powder, lyophilized, for solution |
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
| Labeler - Eugia US LLC (968961354) |
| Establishment | |||
| Name | Address | ID/FEI | Business Operations |
|---|---|---|---|
| TTY Biopharm Company Limited LiouDu Factory | 658742855 | ANALYSIS(55150-365) , STERILIZE(55150-365) , LABEL(55150-365) , MANUFACTURE(55150-365) , PACK(55150-365) | |
More about amphotericin b
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (1)
- Side effects
- Dosage information
- During pregnancy
- Drug class: polyenes
- Breastfeeding
- En español
